April 2021 - Dr. Rebecca Lee Smith
Dr. Rebecca Lee Smith is an Associate Professor of Epidemiology in the Department of Pathobiology at the University of Illinois College of Veterinary Medicine. She also holds affiliate appointments in the Department of Biological and Translational Sciences at the Carle Illinois College of Medicine, the Carl R. Woese Institute for Genomic Biology, the Center for Digital Agriculture, the National Center for Supercomputing Applications, and the Women & Gender in Global Perspectives Program. Dr. Smith heads the Modeling for Disease Control Improvement Lab, which researches everything from disease spread in livestock, to perimenopausal health outcomes, to pathogen risk in reused water. In addition, Dr. Smith is part of the University of Illinois at Urbana-Champaign's SHIELD team that has worked to develop the University's coronavirus testing and tracing protocol over the past year.
From the University Archives
Controlling the spread of infectious disease has always been a problem for universities, and the University of Illinois is no exception. Throughout the twentieth century, the university published numerous reports and informative works to help educate students and staff about disease, provide guidelines for mandatory student testing, and analyze patterns of disease across the university's population.
Tuberculosis was a particularly taxing problem at the University of Illinois, and campus health officials worked hard to curb its spread among students and trace the source of infections. Changes in medical technology, however, made it easier to determine who had been exposed to the tuberculosis bacteria and who had not, even before showing symptoms. In the late 19th century, a German scientist named Robert Koch discovered a protein called tuberculin. While he originally believed this protein could cure tuberculosis, he and other scientists learned that it had far more use in other applications. Over the first decades of the twentieth century, other scientists—such as Charles Mantoux, Clemens von Pirquet, and Florence Seibert—used Koch's breakthrough to develop a new skin test that could accurately diagnose exposure to tuberculosis bacteria within 48-72 hours. By the 1940s and 50s, the United States and the World Health Organization had developed standardized tuberculin proteins and widely used this skin test to determine tuberculosis infections.
In the 1930s, with the economic devastation brought on during the Great Depression, the University of Illinois Health Service issued a report about increased tuberculosis infections on campus. It expressed concern that tuberculosis infections were higher on campus that year than they had been previously, and cited students' lack of regular meals, inadequate sleep, and propensity to overstretch themselves as potential reasons for the uptick in infections. Besides those who had confirmed infections, the university also conducted a survey of students who had a family history of tuberculosis or who lived with a tuberculosis patient. Nearly 8% of the student body, based on these factors, was determined to be at a high risk for infection. In response, the Health Service issued a list of five steps the university should take in order to more accurately assess risk and prevent serious disease from spreading. These steps included taking thorough medical histories of each student, conducting full physical exams before registration, administering the tuberculin skin test (which was becoming more common at other universities, but not yet at Illinois), providing chest x-rays for students who tested positive, and following up with students regularly
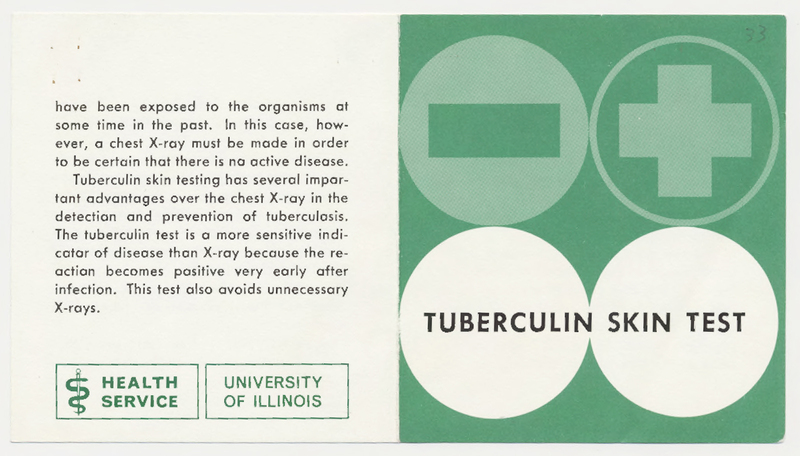
Around the 1940s or 50s, the University of Illinois at Urbana-Champaign required that every new student take the now-standard tuberculin skin test at registration. The University of Illinois Health Service was careful to reiterate to students that positive results did not necessarily mean that the student had tuberculosis. Instead, a positive result meant only that a student had been exposed to the bacteria at some point. Many developed some immunity to the disease and never developed symptoms, but the Health Service mandated that all students who tested positive needed to have a chest x-ray in order to determine if they were infected.
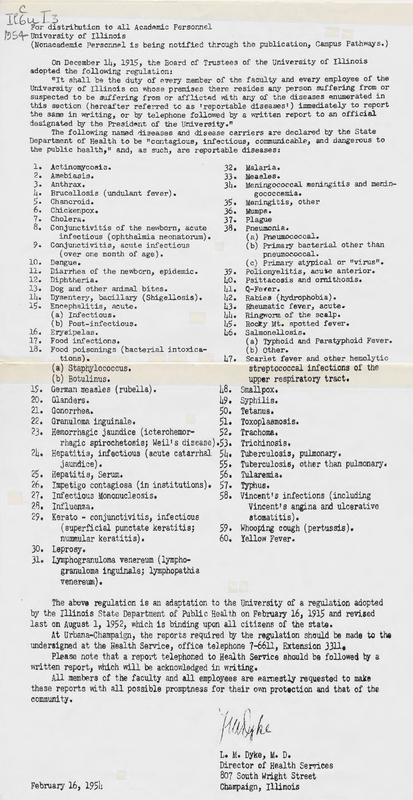
Beginning in 1915, the Board of Trustees at the University of Illinois required faculty and staff to report if they or a member of their household was diagnosed with a particularly dangerous and communicable disease. The Illinois Health Services office regularly updated this list, and by 1954 it included sixty reportable diseases—including leprosy, food poisoning, trachoma, influenza, scarlet fever, and many others. Because the University of Illinois at Urbana-Champaign was, and is, deeply entwined with the surrounding cities of Champaign and Urbana, this policy helped to ensure the public health of the community as well as the university.
The University of Illinois at Urbana-Champaign has long used new testing procedures, measured statistics and modeled risk, and worked with the community to promote good public health outcomes. During the COVID-19 pandemic, Dr. Rebecca Lee Smith and the rest of the SHIELD team have taken similar measures to make campus and the surrouding community as safe and well-managed as possible.
Sources and Futher Reading
Communicable Disease Materials, 1928, University of Illinois Archives
Goldstein, Ellie J.C, Elsie Lee, and Robert S. Holzman. "Evolution and Current Use of the Tuberculin Test." Clinical Infectious Diseases. Volume 34, Issue 3. 1 February 2002. Pages 365–370, https://doi.org/10.1086/338149.